Published April 21, 2022
This National Volunteer Week, we want to recognize our amazing volunteers who work hard to help improve pediatric heart care in underserved communities. Before the pandemic, medical volunteers spent hours traveling to train their peers in person. Currently, they spend multiple hours designing and conducting virtual trainings to continue to make an impact. We asked our global partners why they are grateful for these partnerships.
SÃO PAULO, BRAZIL

Dr. Leonardo Miana, a cardiac surgeon at Instituto do Coração (mentored by SickKids, Canada):
Five years ago, we had the chance to meet the volunteers who would cooperate with us. So naturally, we were apprehensive and enthusiastic about it. We had heard about Dr. Steven Schwartz and Dr. Glen Van Arsdell from SickKids, but we didn’t know what to expect.
They spent a couple of days with us, listening to our presentations, taking part in quick rounds, and watching one surgery. At first, I thought it was a short time for them to acknowledge our reality. When I was driving Dr. Schwartz and Dr. Van Arsdell to the airport, I listened to them talking about their first impressions. I was very impressed by how they could realize so much in such a short period!
A lot has taken place during these five years, but I can tell that what impressed me the most was how they cared about our program as if they were part of it. And, in fact, they are. Even from a distance, they really look after our patients and do their best to improve our knowledge and outcomes.
We struggled to keep in touch during the pandemic, and virtual meetings came in handy. Nevertheless, we can’t wait to experience in-person visits again. It will be a reassuring experience when they see with their own eyes how everything is changing for the best with their support.
QINGDAO, CHINA
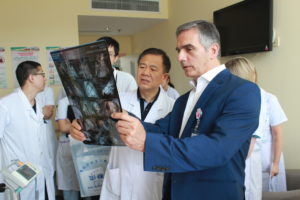
Dr. Chen Rui, a cardiac surgeon at Qingdao Women and Children’s Hospital (mentored by Alder Hey Children’s Hospital, England):
I sincerely appreciate having had the opportunity to briefly work with Dr. Rafael Guerrero’s team from Alder Hey Children’s Hospital, which is a wonderful physician volunteer team and very helpful for us. Every member of the team shared his or her time and talents with us and provided hand-in-hand education and training. It’s included a wide variety of knowledge: physiology and pathology of complex congenital heart disease, preoperative patient evaluation and preparation, surgical indication and skills, anesthesia and cardiopulmonary bypass, patient transfer process, postoperative care, functioning of a multidisciplinary team, and nursing. There were some positive changes at the hospital in each of the above subjects. I am very grateful to Dr. Rafa’s team and their wonderful volunteer work.
COVID has affected our face-to-face communication. I hope that in near future, we will have the continuous opportunity to accept training from Dr. Rafa’s team, particularly on family care of patients with congenital heart disease, surgical skills, postoperative care of complex congenital heart disease in neonates, and postoperative follow-up.
KUALA LUMPUR, MALAYSIA

Dr. Sivakumar Sivalingam, a cardiac surgeon at Children’s HeartLink Center of Excellence Institut Jantung Negara (mentored by Birmingham Children’s Hospital, England):
The medical volunteers that visited our cardiac unit were from world-renowned cardiac centers. My favorite memory of these partnerships was the excellent teamwork and bond that was built between the two teams. This bond enabled us to break the barrier and gave us a feeling that the volunteer team was a part of us. I believe that this kind of strong bond is very important for a successful collaborative program.
We were able to work together in a very amicable environment. The dedication and commitment of medical volunteers to high-quality care inspired our team to follow a similar ethos, and it has inspired us to help the other teams within the country to achieve high standards of care. During their visits, we sometimes had very challenging patient cases in which our team expected that the treatment would have a futile effort. But the sheer dedication and perseverance of medical volunteers helped us have successful results. These attributes certainly inspired our team to provide high-quality care for our patients.
Our partners made us realize that in order to provide such high-quality care, we need to adopt a practice based on teamwork rather than individual care. This practice made us extend our training not only to the physicians but also to the paramedical staff to empower them in the care of the patients.
The volunteer teams had completely taken our unit on a different trajectory. Before that, we provided care only for simple congenital heart diseases. With these partnerships, we are now able to provide high-quality care even for complex congenital heart lesions. We would like to thank the volunteer teams for helping us achieve the status of the Children’s HeartLink Center of Excellence. After a brief hiatus, we are looking forward to learning from Children’s HeartLink about aspects beyond the care of patients — such as quality improvement initiatives, education, research and training.
HO CHI MINH CITY, VIETNAM
Dr. Chau Nguyen, a pediatric cardiac intensivist at Nhi Dong 1 (mentored by Gleneagles Hospital, Singapore, and Boston Children’s Hospital, USA):
Looking back on our almost 15-year pathway with Children’s HeartLink, I think of many medical volunteers who have been willing to donate their time, expertise and talents to help support our team. During this Volunteer Recognition Week, I would like to thank all of them for the outstanding job that they did at our CICU.
What is my favorite memory about medical volunteers? I want to share about two volunteers under the connection of Children’s HeartLink whose wonderful work has made a big change in our cardiac unit.
Mary Tan, a teaching nurse from the National University of Singapore, did a lot of training for our ICU nurses from 2009 to 2014. I remember when she first came to our hospital in 2009 observing our limited resources and lack of trained personnel, she told me that she would like to do a project on the ICU nurse training. What touched me the most was the compassion she showed to the patients we served. After listening to our ICU’s problems and conflicts at that time, she had promised to help me train my nurses until I felt comfortable and confident doing my duty at night. We together did three basic trainings and then two advanced courses every year. She did the training and I did an interpretation. Our nurses really responded to her and felt happy every time she came to us. That’s probably due to how patient she was with them. I could see their nursing skills and nursing assessments improving and their confidence growing with each session she did. Our nurses were so lucky to have her as a tutor and so we are. Thank you so much, my dear friend, Mary.

Beverly Small, a head nurse of CICU at Boston Children’s Hospital, has become not only our nurses’ teacher but also our “idol.” She helped change our perception of life and work. When Beverly first came to our cardiac unit and saw that children treated in the ICU were unable to see their mothers due to our visitor policies, her heart was broken. She showed us many scientific studies regarding the benefits of the presence of family members in the ICU on the recovery of the patients. Previously, we only thought of the physical health of the patients and tried to struggle for their survival. We unintentionally forgot about psychological challenges for patients and their family members. The majority of nurses had wrong beliefs such as the intervention of family and the increased risk of infection. This wrong perception was gradually changed. Nowadays, our nurses’ attitude toward family members has been improved dramatically. They understand the severe stress and worry that the parents and their kids experience in the ICU after a cardiac operation. They facilitate the longer presence of family members and their participation in care for their children. They also remind doctors to respect the visiting time and explain the patient condition during this time.
Because of the pandemic, we are unable to see Beverly in person. She always takes part in Zoom meetings to know our ICU progress. We really miss her and wish to see her here again as soon as possible.
COIMBATORE, INDIA

Dr. Kaushik Jothinath, an anesthesiologist and intensivist at G. Kuppuswamy Naidu Memorial Hospital (mentored by Mayo Clinic, USA):
As medical professionals, all of us strive to “find the next gear.” I think being in constant touch with the volunteer team from Mayo Clinic – Dr. Mike Nemergut, Dr. Grace Arteaga and Dr. Joseph Dearani – has helped us raise the bar and increase the standard of care being given to children with heart disease in this part of the world.
I want to share a few experiences which I had with the Mayo team and particularly with an anesthesiologist Dr. Mike Nemergut. This will definitely demonstrate how he has inspired me and influenced my perspective on taking care of children undergoing corrective cardiac surgery. In December 2018, I had my onsite visit to Mayo Clinic in Rochester, Minnesota. Being my first time outside the country, I had some jitters. However, this was only until I stepped into the Mayo Clinic campus. Once I was in, Dr. Mike personally accompanied me and made sure that I was in safe hands. I was touched by his gesture and humility. Regardless of his busy O.R. schedule on that day, he took up my comfort as an additional responsibility as he dropped in from time to time to check on me. Even though I stayed in Mayo only for six days, Dr. Mike ensured that I spent each day with a different anesthetist so that I could get a different perspective from each person, spend my time fruitfully and exchange my ideas. This taught me a valuable lesson about time. Whether it is yours or someone else’s, it should always be respected.
Before that instance, Dr. Mike was presenting a lecture in Coimbatore during the partner site visit in 2017. While explaining the association between uncuffed tube and stridor, he used an analogy. He explained how many dying people have grey hair. This does not imply that grey hair causes death. It simply means as an old man, you are at a higher risk of dying. The clarity of thought and choice of a parallel explanation to drive home his point inspired me to have the same clarity of thought while expressing ideas for public consumption. I have ever since made an earnest attempt to keep my presentations crisp and to the point so that the prime idea is conveyed in no uncertain terms.
During my partner site visit to Mayo Clinic, while working with Dr. Devon Aganga we were doing redo tricuspid valve replacement surgery for a post-Fontan patient. This patient would have been ventilated typically in our set-up. However, Dr. Aganga ended up extubating the patient on the table. This conveyed a very important message: if a patient is doing well and surgery has gone on uneventfully, on-table extubation should definitely be considered for every patient. This was a drastic change in perspective, and we have since developed our own program and protocol to ensure the same.
There is only one thing I would like to say: A BIG THANK YOU!!!
The Children’s HeartLink staff is sharing their appreciation of the volunteers.
